Lipid Accumulation in Microglia Contributes to Neuroinflammation and Neurodegeneration
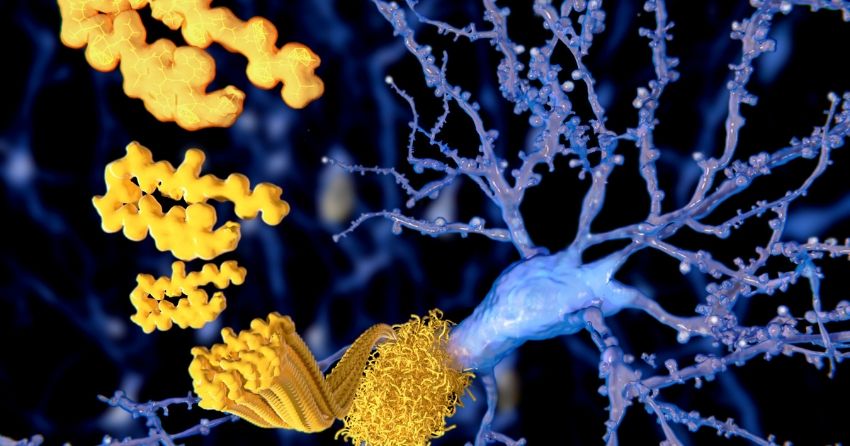
Researchers have found that microglia in the aging brain have a tendency to accumulate lipids, and that those that do are harmful. This is a fascinating discovery, given that microglia are essentially the central nervous system version of macrophages elsewhere in the body, and lipid accumulation in macrophages leading to senescence and inflammatory behavior is an important mechanism in atherosclerosis. Further, it is well established that microglia in the brain become inflammatory, senescent, and dysfunctional in later life, and this behavior contributes to the progression of neurodegenerative conditions. It has been demonstrated that removing senescent microglia can turn back Alzheimer's pathology in mouse models of the condition, for example. This lipid accumulation might be an important aspect of dysfunction in microglia, though it is anyone's guess at this point as to where it sits in the web of cause and effect.
Article first published on FightAging.org
Microglia in the brain assume a dizzying array of states. Now researchers describe a new one: lipid droplet-accumulating microglia (LAM). These lipid-stuffed cells resemble the foamy macrophages seen in atherosclerotic lesions. They accumulate in the hippocampus of the aging brain and appear to be bad news, hiking inflammation and reactive oxygen species while having little ability to phagocytose debris. Notably, inflammatory stimuli induce LAM, as do some genetic variants associated with neurodegenerative disease.
Previous studies have identified a smorgasbord of distinct transcriptional profiles delineating subtypes of microglial states. A handful of these have been correlated with neurodegenerative disease. These include disease-associated microglia (DAM), which cluster around plaques in mouse models of amyloidosis, and the similar microglial neurodegenerative phenotype (MGnD) found in multiple mouse disease models. A recent study characterized human Alzheimer's microglia (HAM), which were isolated from the Alzheimer's brain. It is still unclear how all these types relate to each other and what they do.
While examining hippocampal sections from aged wild-type mice by electron microscopy, researchers were struck by the accumulation of lipid droplets inside microglia. These microglia resembled cells first described by Alois Alzheimer, who reported lipid-stuffed glia clustering around amyloid plaques in the Alzheimer's brain more than 100 years ago. Researchers quantified the phenomenon in mice, finding that more than half the hippocampal microglia in 20-month-old wild-type animals contained from one to three lipid droplets. Droplets were rare in other brain regions, and nearly absent in 3-month-old mice.
To characterize these LAM, the authors isolated microglia from aged mouse hippocampi and sorted out those with high lipid content. Transcriptional profiling revealed 692 genes that were differently expressed between cells with low and high lipid content. In particular, genes involved in the production of reactive oxygen species, lipids, and pro-inflammatory cytokines were up in LAM, while genes responsible for phagocytosis were down. Notably, this transcriptional profile was in many respects the opposite of DAM, which turn up phagocytotic genes.
Functional studies of LAM reinforced these transcriptional findings. When the authors injected myelin debris into aged mouse hippocampus, microglia without lipid droplets engulfed it, but few LAM did. LAM isolated from brain produced more reactive oxygen species (ROS) than did low-lipid microglia, and they secreted higher levels of several pro-inflammatory cytokines such as CCL3, CXCL10, and IL-6. How do these cells arise? Because many of the LAM genes are regulated by inflammation, researchers speculate that they are products of an inflammatory response.