Killer T-Cell Build-Up in the Brain Leads to Cognitive Decline in Older Age
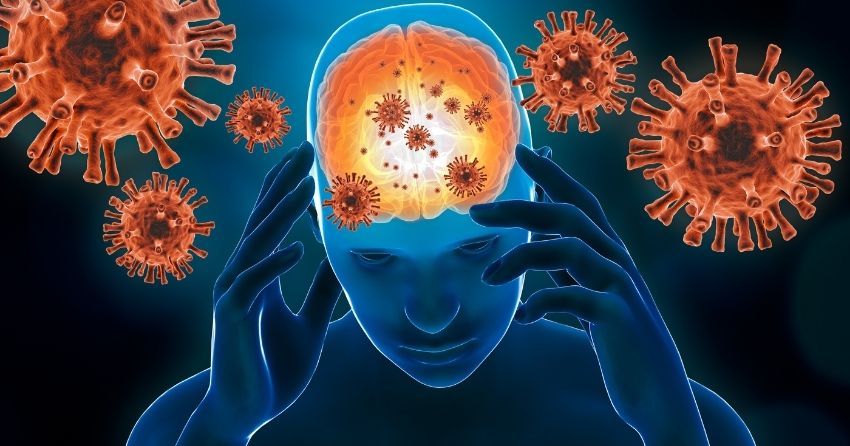
The central nervous system — the brain and spinal cord — is prone to decline as we age. Besides chronic disease and trauma, the immune system plays a part in how nervous structures become damaged over time.
Now, a research team from the University Hospital of Würzburg in Germany set out to identify the steps that are involved in the chronic inflammatory response that leads to neuronal damage. A recent study published in the journal Nature Aging sheds some light on how the process works. The study shows that the accumulation of CD8 T-Cells is one of the primary culprits in a series of events that lead to neuronal damage (1).
The Brain Is Susceptible to Damage From Inflammation
A specialized type of immune cell that is present in the central nervous system is the cytotoxic CD8 T lymphocyte. Also called killer T-cells, they protect tissues from threats like bacteria and viruses.
But, excessive activity by killer T-cells may damage the very structures that they are meant to protect. In certain cases, these cells can’t distinguish between outside threats and the body’s tissues, causing damage to healthy tissue. This type of self-induced damage is the basis for autoimmune disorders that affect the nervous system, like multiple sclerosis.
It is this very type of collateral damage caused by excessive immune responses that may play an important role in the deterioration seen in aging. As we get older, T-cells accumulate in the central nervous system from previous immune responses. Although these cells are no longer fighting any active threats, they continue to exert an inflammatory response that has damaging effects on the surrounding tissues.
Previous studies have shown that chronic inflammation of nervous tissue, or neuroinflammation, can lead to cognitive decline in older age (4). Neuroinflammation also plays an important role in the development of certain types of dementia, such as Alzheimer’s disease (5).
So, why is the central nervous system so very susceptible to damage mediated by inflammation? A special sheath called myelin that covers the projections of neurons is especially sensitive to neuroinflammation. Without this special, conductive tape-like covering, neurons can’t send signals between themselves through their projections called axons. This type of damage can lead to cognitive defects as well as sensory issues and difficulty with movement.

Migrating T-Cells Accumulate in the Aging Mouse Brain
In their research article, the German team of researchers identified the over-activation of immune cells in the central nervous system to be the issue that triggers chronic inflammation, and aged cells are more susceptible to being damaged.
Using aged mice to observe how the events of the inflammatory response unfold in real-time, the researchers observed that killer T-cells were present in large numbers in the brains of aged mice. Groh and colleagues showed that an accumulation of CD8+ T-cells drives degeneration of axons — the myelin-covered projections that connect neurons — in the normal aging mouse central nervous system and contributes to age-related cognitive and motor decline.
In addition, they found that distant sites in the body can activate these immune cells — and not just when there is a need for protection from within the central nervous system itself. Immune threats from outside of the central nervous system were activating CD8 T-cells, leading to their accumulation.
“We show that the accumulation of CD8+ T cells leads to degeneration of nerve fibers in the central nervous system of normal aging mice, which contributes to motor and cognitive decline,” said the principal author Dr. Janos Groh. “In addition, we show that T cell-mediated damage in aged but not adult mice is aggravated by systemic inflammation".
Killer T-Cells Flood the Aging Human Brain
Now, the real question is, does this apply to us? To do so, Groh and colleagues investigated brain autopsy samples from adult (25- to 50-year-old) and older (over 70 years) humans without neurological disease. In white matter autopsy material from older humans, Groh and colleagues also found increased densities of T cells.
“These observations suggest that even in humans, CD8+ T lymphocytes might contribute to axonal perturbation and dysfunction in the aging central nervous system,” concluded the researchers. “‘Our results suggest that targeting CD8+ central nervous system-associated T cells in older adults might mitigate aging-related decline of brain structure and function.”

Paving the Way for Preventing and Treating Neuroinflammation
The study shows the robust impact of CD8+ T cells in the normal aging brain, and that naturally occurring inflammation makes the aging brain susceptible to additional damage by infection-related systemic stimuli.
This sets the stage for future research to work on the development of strategies for prevention and treatment. The key now is to take a more in-depth look at the process to clarify why and how the body initiates this inflammatory response.
References:- Groh, J., Knöpper, K., Arampatzi, P. et al. Accumulation of cytotoxic T cells in the aged CNS leads to axon degeneration and contributes to cognitive and motor decline. Nat Aging 1, 357–367 (2021). https://doi.org/10.1038/s43587-021-00049-z
- Yuan X, Klein D, Kerscher S, et al. Macrophage Depletion Ameliorates Peripheral Neuropathy in Aging Mice. J Neurosci. 2018;38(19):4610-4620. doi:10.1523/JNEUROSCI.3030-17.2018
- Groh J, Martini R. Neuroinflammation as modifier of genetically caused neurological disorders of the central nervous system: Understanding pathogenesis and chances for treatment. Glia. 2017;65(9):1407-1422. doi:10.1002/glia.23162
- Bowman GL, Dayon L, Kirkland R, et al. Blood-brain barrier breakdown, neuroinflammation, and cognitive decline in older adults [published correction appears in Alzheimers Dement. 2019 Feb;15(2):319]. Alzheimers Dement. 2018;14(12):1640-1650. doi:10.1016/j.jalz.2018.06.2857
- Calsolaro V, Edison P. Neuroinflammation in Alzheimer's disease: Current evidence and future directions. Alzheimers Dement. 2016;12(6):719-732. doi:10.1016/j.jalz.2016.02.010